
It was a privilege to present at the recent Next Generation Patient Experience conference. I had never attended a conference solely focused on healthcare, so I learned a lot about what innovative healthcare systems are doing to improve the patient experience.
There are definite best practices, but there are still a lot of unknowns. Healthcare is just catching up to the idea they are competing in a consumer-driven culture. The old way of doing things just isn’t going to work for much longer.
It was truly inspiring to hear doctors, executives and caretakers of all kinds discuss what’s important to patients. Here are a few themes:
This is the word used regarding scheduling and geography and everything in between. How accessible is healthcare?
From a customer experience perspective, I couldn’t help but wonder if they consider things like customer effort score. When I try to call for an appointment, why do I have to call on their terms? Why can’t I schedule via a mobile app? Some providers are starting to offer convenience like this, but it certainly isn’t the norm yet.
Empathy in healthcare is the now frontier. Access is part of empathy. #NGPX via Dr. Boissey from @clevelandclinic
— Jeannie Walters (@jeanniecw) December 2, 2015

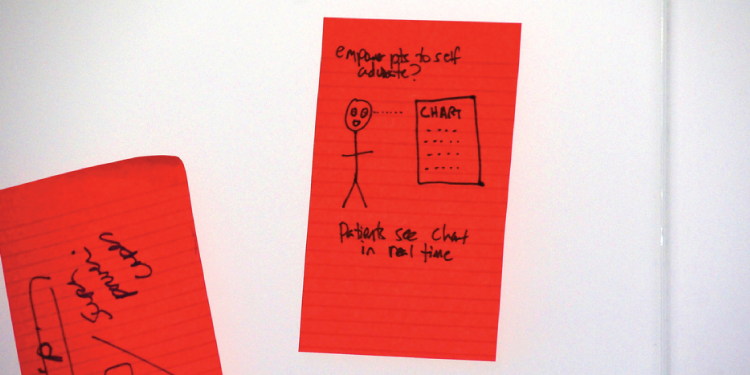
Giving both doctors and patients tools to share information this way is on the rise. But the concern is how to use these tools without losing the person-to-person interactions which are so critical. Doctors raved about having mobile tablets to receive and react to real-time information, but patients require education about how they are used. Perception is reality, and if the patient perceives caretakers using tablets or mobile devices as a distraction to care, they simply won’t work.
65% of health care transactions will be mobile by 2018 #ngpx — Randi Redmond Oster (@helpme_health) December 2, 2015
The best experiences are always linked to people. But what if a physician doesn’t understand how his or her body language can impact the way a patient perceives their experience? These are the questions being dealt with now.
One of my favorite examples was using video to show doctors and nurses how they were really behaving. Of course there were things they didn’t “see” until they reviewed their interactions on video.
Just like any organization, culture is king in healthcare organizations. If every employee is driven by avoiding punishment instead of doing what’s right for the patient they are serving, the experience of everyone will suffer.
Many organizations now have patient and family advisory councils. These groups provide feedback on everything from how often should a new mom be interrupted in her room to what’s the most compassionate way to share that a loved one has died. They have a voice that is heard by the people who need to hear it.
It’s enlightening to hear what the leaders in this space are tackling. Nurses and others deal with “compassion fatigue.” Some specialties have a high rate of doctor burnout. As new electronic and digital solutions are incorporated into their workflows, the most experienced workers can feel left behind and incompetent.
It’s not easy. But it’s truly important to see the results we all want to see. If we, as patients, experience compassionate care and feel seen and heard, we experience better outcomes in our overall health.
Yes, healthcare has a ways to go in their patient experience work. But I’m very encouraged by what I am seeing and proud to be a very small part of it.
Image credits: Amy the Nurse, Tai Chiahung, tedeytan via Creative Commons license
 Jeannie is an award-winning customer experience expert, international keynote speaker, and sought-after business coach who is trailblazing the movement from “Reactive Customer Service” to “Proactive Customer and Employee Experience.” More than 500,000 people have learned from her CX courses on LinkedIn Learning, and her insights have been featured in Forbes, The Chicago Tribune, The Wall Street Journal and NPR.
Get Jeannie’s insights in your inbox each week by subscribing to The Weekly Win and follow her on LinkedIn, Instagram and YouTube.
Jeannie is an award-winning customer experience expert, international keynote speaker, and sought-after business coach who is trailblazing the movement from “Reactive Customer Service” to “Proactive Customer and Employee Experience.” More than 500,000 people have learned from her CX courses on LinkedIn Learning, and her insights have been featured in Forbes, The Chicago Tribune, The Wall Street Journal and NPR.
Get Jeannie’s insights in your inbox each week by subscribing to The Weekly Win and follow her on LinkedIn, Instagram and YouTube.